Day 2 :
Keynote Forum
Peter P Karpawich
Wayne State University, USA
Keynote: Congenital /structural heart into the 21st century: Advances in diagnosis and intervention
Time : 09:05-09:30

Biography:
Abstract:
A repaired congenital heart defect (CHD) does not equate to a normal heart. With time, residual or new patient (pt) age-related issues including valve stenosis or insufficiency, changes in vessel dimensions, stunts, and arrhythmias will require continued intervention and medical management. Early heart failure, based solely on cardiac anatomy, remains an important concern for which there are evolving therapies. The newly coined term, ”Structural Heart” as it applies to valve and vessel issues, other than coronary arteries, often is only a substitute term for CHD among older patients. At the current time, there are about 2 million pts > 18 years of age in North America and Europe alone, with repaired CHD. A number far greater than children with CHD. The recognition of this increasing and evolving patient population data base has prompted the American Board of Internal Medicine to create a new sub-specialty training program and Board examination in Adult Congenital Heart Disease (ACHD). Comparable recognition in England utilizes their Grown-up Congenital Heart (GUCH) programs. The purpose of this presentation is to identify the scope of the problem facing clinicians today and to illustrate current advances in recognition and therapy.
In the field of anatomical diagnosis, non-invasive imaging now includes standard 2D and 3D ECHO/Doppler studies as well as MRI/CT scans. Recently, physicians have been aided by the development of 3D printed soft tissue models of precise. Considering the complexity of certain repaired CHD, these precise anatomical models allow pre-operative planning and familiarization with cardiac/vascular structures as well as patient education. Since repeat open thoracotomies are often technically challenging, expensive as well as associated with high patient morbidities, non-surgical interventions have been greatly aided by use of vascular-accessed devices to open stenotic valves and vessels by use of various balloon catheters or stents, both covered and expandable. A major paradigm shift has evolved over the past ten years with more interventional cardiac catheterization laboratory procedures now being performed indeference to repeat surgical operations. At present, about 70% of residual CHD problems are now be amenable to interventional catheterizations, including insertion of valves.
Certain CHD may intrinsically predispose to arrhythmias and the addition of prior surgical operations leaves residual scars which only augment the arrhythmia burden among CHD pts. Ablation mapping with non-fluoroscopic techniques has greatly reduced radiation exposure to patients and catheterization lab personnel. Non-fluoroscopic procedures eliminate the need for lead aprons, which decreases orthopedic problems commonly seen among electrophysiologists and lab technicians. Although not included in current published “guidelines’, resynchronization pacing for heart failure has been applied to CHD pts with variable success.om
ACHD is an evolving field and will continue to expand as more children survive to adulthood from what previously had been fatal heart defects due to improvements in interventional procedures. Continued knowledge and awareness in the field will be required by all involved in patient care.
- Interventional Cardiology | Coronary Heart Diseases | Cardiac Surgery
Location: Madrid, Spain

Chair
Hatem AlMasri
King Abdulaziz Medical City, Saudi Arabia
Session Introduction
Hatem AlMasri
King Abdulaziz Medical City, Saudi Arabia
Title: Correction using surgical procedure of tetralogy of fallot with small pulmonary annulus – Can we preserve the valve annulus
Time : 09:30-10:00

Biography:
Dr. Hatem Al-Masri is a cardiac critical care intensivist and consultant of cardiac surgery. Dr. Al-Masri completed his medical degree (M.D.-Doktorate(PhD) at Charles University – Faculty of Medicine, holds a degree in biochemistry from the University of Waterloo - Canada, completed his residency training in Germany (Leading Facharzt) and holds training fellowships in Cardiac Surgery from IJN, KL, Malaysia, Switzerland, and Canada. Dr. Al-Masri is the author of an award-wining medical research paper titled “Hemodynamic Support Requires Integrated Approach Comparing LVAD vs. IABP in Patients Experiencing Left Venticular Failure” (Best Paper of Young Cardiac Surgeon) at the 8th International Congress of Update in Cardiology and Cardiovascular Surgery (UCCVS 2012) awarded by European Society for Cardiovascular Surgery, World Society of Arrhythmias (WSA ) and the Society of Cardiology and the International Academic of Vascular and Endovascular Surgery (ISCP). Dr. Al-Masri is a member of the Medical German Association, Malaysian Medical Association and the Saudi Medical Council.
Abstract:
To determine the outcome of repair of Tetralogy of Fallot (TOF) with small pulmonary annulus by preserving the pulmonary valve.
All consecutive patients (n=41) operated by a single surgeon using the above technique were reviewed. The pulmonary annular size was based on preoperative transthoracic or intraoperative TEE measurement. All patients had pulmonary annular size with Z value of -2 or less.The mean age of the patients were 6.2 years (range from 2 to 23). There were more males to females (26:15). All patients were cyanosed, and 11 were severely cyanosed. Eleven patients had previous Blalock-Taussig shunts, with 2 patients had 2 shunts done. The mean Z score of the pulmonary valve annulus was Z – 4.3 +/- 1.69 mm. All patients had bicuspid and/or dysplastic pulmonary valve. All except 4 patients had infundibular and pulmonary artery augmentation. Post correction mean RV/LV pressure ratio was 0.83. The mean pulmonary valve gradient was 34.8 mmHg. The mean cardiopulmonary bypass time was 143 min and the mean cross-clamp time was 77 min. The mean extubation time was 27 hours and mean ICU stay was 48 hours. All except 4 patients had either none or mild pulmonary regurgitation. There was only 1 mortality in this series. Serial echocardiography was done on follow up. The longest follow up is 3 years and all patients who survive are currently doing well.
The preservation of the pulmonary valve in
Peter P. Karpawich
Wayne State University, USA
Title: When the guidelines don't apply: Contractility (dp/dt-max)-guided resynchronization pacing among patients with congenital heart and heart failure
Time : 10:00-10:30

Biography:
Dr Karpawich completed his Masters in Science degree from The University of Detroit and his Medical Degree from Hahnemann/Drexel University in Philadelphia, PA. His postdoctoral Residency in Pediatrics at The Children's Medical Center, University of Texas (Dallas), and Pediatric Cardiology Fellowship at Texas Children's Hospital, Baylor University (Houston). He founded and is Director of the Cardiac Electrophysiology Program at the Children's Hospital of Michigan and Professor of Pediatric Medicine, Wayne State University School of Medicine (Detroit). He has published over 200 scientific papers, textbook chapters and textbooks typically in the field of cardiac electrophysiology, pacing and heart failure management both in children and adults with congenital heart disease, and is on the editorial staff of several internationally-recognized medical journals.
Abstract:
Objectives: Patients (pts) with repaired congenital heart disease (CHD) can later develop heart failure (HF), leading to heart transplant (HT). Although cardiac resynchronization pacing therapy (CRT) has been applied to pts with normal anatomy, there is little information on CRT and CHD. This study evaluated acute hemodynamic contractility (dP/dt), not guidelines, among CHD pts to determine if it can predict chronic CRT efficacy.
Methods: Forty pts with CHD and HF (NYHA II-IV) underwent cardiac catheterization (cath) with dP/dt-max both before and after acute CRT pacing. If acute paced-dP/dt-max improved ≥ 15% from baseline with CRT pacing, pts were given the option of CRT. Clinical follow-up after CRT testing was from 2-144 months (mean 35).
Results: Preexisting pacemakers were present in 70% of pts. CHD was variable with 16/40 (40%) pts having either a single or systemic “right” ventricle morphology. Of the 40 pts, 26 (mean age 22y) met criteria for CRT benefit while 14 (mean age 29y) did not. There were no differences in age, QRS duration, left ventricular (LV) ejection fraction, LV end diastolic diameter, V contractility (dP/dt-max), nor PM between CRT groups. Among the CRT recipients, 21 pts (81%) improved in NYHA class and were removed from HT consideration. All underwent a repeat cath 6-14 months later showing continued improved contractility.
Conclusion: Since published CRT guidelines do not apply to CHD pts, a better way to select which CHD pts may benefit from CRT is needed. Pre-CRT testing by direct paced-contractility response improve patient selection and responder rates.
Ygal Plakht
Ben-Gurion University, Israel
Title: Acute MyoK+ardial Infarction: The association of changes in K+ levels and in-hospital mortality of patients with acute myocardial infarction
Time : 10:45-11:15
Biography:
To be updated soon...
Abstract:
Background: Serum potassium levels (K, mEq/L) of patients with acute myocardial infarction (AMI) were found to be associated with short- and long-term outcomes. Nevertheless, significant fluctuations in K have been reported during the acute phase of an AMI.
Aims: To evaluate the association between K changes during the hospitalization and in-hospital mortality of patients admitted with AMI.
Methods: AMI patients hospitalized in a tertiary medical center, between 2002-2012, for 3 days or longer, were studied. Based on K levels during the hospitalization, the following parameters were calculated: minimal, maximal, range (maximal-minimal) and fluctuation (the gap between two consecutive K levels). The latter parameters were calculated for every K throughout the hospitalization. The associations between the parameters and outcome were assessed using generalized estimating equations model, adjusted to baseline patients’ characteristics and results of other routine laboratory tests (i.e. Sodium, Creatinine and Glucose).
Results: Overall 16,596 admissions of 12,176 patients were included (age 67.8±13.9 years, 66.6% males), and 111,457 K results registered. Overall, patients discharged alive from 15,564 admissions, with an in-hospital mortality rate of 6.2%. Compared with survivors, in-hospital mortalities had higher mean K (4.4±0.8 vs. 4.3±0.6), higher rate of fluctuation or range ≥0.4 (p<0.001 for each). Minimal K throughout the first 48 hours was significantly more prevalent among survivors compared to deceased (41% vs 25% p<0.001). In a multivariate analysis the following parameters were found to be independent prognostic marker for mortality: K<3.9 (adjOR=1.22) or K>4.8 (adjOR=1.17), range ≥0.8 (adjOR=1.53) and minimal K during the first 2 days of admission (adjOR=1.49). Furthermore K fluctuation ≥0.4 was associated with increased mortality within the following 72 hours (adjOR=1.37), (p<0.001 for each).
Conclusions: changes in K, in addition to extreme values throughout an admission of AMI patients are strong prognostic markers of in-hospital mortality. Close monitoring of K in addition to further evaluation of mechanisms and interventions in K are in order.
Imtiaz Ahmed Chaudhry
Armed Forces Institute of Cardiology and National Institute of Heart Disease, Pakistan
Title: Effectiveness of maximum functional capacity (VO2 Max): an assessment tool for preoperative suitability in cardiac surgery. A descriptive cross sectional study from Pakistan
Time : 11:15-11:45

Biography:
Dr Imtiaz Ahmed Chaudhry did his Fellowship in General Surgery in 2004, and later completed his second Fellowship in Cardiac Surgery from College of Physicians and Surgeons, Pakistan in 2011. He completed one year training (IMGSS) in Cardiothoracic Surgery at Queen Elizabeth Hospital Birmingham UK, in 2013.
He is working as a consultant cardiac surgeon at Armed Forces Institute of Cardiology and National Institute of Heart Diseases, Rawalpindi, Pakistan.
He is a member of Research Department, Institutional Ethical Review Board and in charge of Adult Cardiac Surgery Database. He has published more than 10 papers in reputed scientific journals.
Abstract:
Objective: There has been an increase in the number of cardiac surgeries, and there is a growing need to predict the morbidity, mortality and quality of life in patients following such surgery. According to recent studies preoperative identification of patients at risk of postoperative cardiac complications is readily achievable using noninvasive cardiopulmonary exercise testing (CPET). This study evaluated the value of VO2 max testing in the preoperative assessment of patients undergoing elective cardiac surgery and whether poor preoperative cardiopulmonary reserve and comorbid state dictate high risk status and predict complications in patients undergoing elective cardiac surgery.
Methods: A descriptive cross sectional study is being carried out at Armed Forces Institute of Cardiology and National Institute of Heart disease, Rawalpindi, Pakistan. All the patients undergoing elective CABG surgery were included according to inclusion criteria. Data were collected on functional status, postoperative complications, and survival.
Results: Initial analysis revealed a mean age of 52 years ± 10.37 and majority of male patients with a mean BMI of 25.1±. Mean VO2 max at admission was 13.6±4.3 whereas VeO2 and VeCO2 were (46.7±25.4) (30.1±15.72) respectively. Postoperatively our cohort of patients had a mean ICU stay of (54.4 hrs±58.09) and ventilation time of 5.3hrs±4.38. Majority of the patients were weaned off with mild inotropes and only one patient had peroperative IABP insertion. In our study preoperative VO2max cardiopulmonary status positively correlates with postoperative prolonged ICU stay and ventilation time at pearson coefficient r=0.422, r=0.485.
Conclusion: CPET is a useful adjunctive test for predicting postoperative outcome in patients being assessed for cardiac surgery.
Maria Kalliopi Konstantinidou
Royal Brompton and Harefield NHS Trust, UK
Title: TLR-4, CD14 polymorphisms and plasma concentration of Soluble CD14; is there a genetic link with Coronary Artery Disease?
Time : 11:45-12:15

Biography:
Ms Maria Kalliopi Konstantinidou studied at the Medical University of Crete with a Scholarship to Boston University. Subsequently she got involved in research at the University of Athens and completed her PhD, which focused on the genetic predisposition to coronary artery disease, as well as a Masters degree in Thoracic Oncology. Having concluded her cardiothoracic surgery training, in hospitals both in Greece and the UK, she is currently a Clinical Fellow in Cardiothoracic Surgery at Royal Brompton and Harefield NHS Trust in London. Ms Konstantinidou has continued to be active in research co-writing and publishing a number of articles.
Abstract:
Background: Inflammatory mechanisms have a key role in the pathogenesis of atherosclerosis. The most frequent functional polymorphisms of TLR-4- Asp299Gly and Thr399Ile- and of CD14 promoter area - C260T polymorphism- are studied in patients with coronary atheromatosis. Plasma levels of soluble CD14 are checked for possible correlation with the severity of Coronary Artery Disease (CAD).
Methods: DNA was obtained from 100 human paraffin-embedded aortic specimens, from cadavers with known coronary atheromatosis (Group A) and 100 blood samples from patients with CAD, as detected by cardiac Multi-Detector-row-Computed-Tomography (MDCT) (Group B). Our control group consisted of 100 healthy individuals (Group C). Genotyping was performed by Restriction Fragment Length Polymorphism-Polymerase Chain Reaction (RFLP-PCR). Plasma levels of sCD14 were measured with ELISA.
Results: For TLR-4 Asp299Gly and Thr399Ile polymorphisms, no statistically significant differences were observed. Regarding the C260T polymorphism, frequencies of T allele were significantly higher in the control group compared to the case group (p = 0.05). The Odds Ratio (OR) showed statistically significant association of TT genotype with healthy individuals (OR= 0.25, 95% Confidence Interval (CI) = 0.10–0.62, p = 0.0017). Plasma levels of sCD14 in patients with CAD (mean value = 1.35 μg/ml) were reduced when compared to reference value.
Conclusions: The studied polymorphisms of TLR-4 showed no association with CAD. Conversely, the studied functional polymorphism of CD14 has a statistically significant difference in expression between healthy and affected by CAD individuals. Further studies could prove the use of sCD14 as possible biomarker for severe coronary disease.
Interventional Cardiology | Coronary Heart Diseases | Cardiovascular Surgery
Farrah Pervaiz
Armed Forces Institute of Cardiology and National Institute of Heart Disease, Pakistan
Title: Reducing surgical site infections through quality improvement initiative: A tertiary cardiac care facility experience in a developing country
Time : 12:15-12:45

Biography:
Dr Farrah Pervaiz has completed her Masters in Public Health from Quaid e Azam University, Islamabad, Pakistan in 2012. Although, a clinician at genes, possesses a special interest in cardiac research, especially clinical / outcomes based research in order to make everyday medicine more up to date and beneficial to the patients.
She is currently working as Director Research and Development department AFIC/NIHD Rawalpindi. She is the founder member of Research Department and Institutional Ethical Review Board.She is also supervising master thesis and has been a research coordinator for national and international clinical trials. Her Research work is extensively disseminated through more than 50 peer reviewed publications in both National and International Scientific Journals.
Her thesis work has been recently published in British Medical Journal and has been an author of many national publications.
Abstract:
Amongst healthcare associated infections (HAIs), surgical site infections (SSIs) are a preventable cause of increased morbidity and mortality and are associated with substantial financial costs. SSI rates are an indicator of the quality of surgical and postoperative care, which necessitates the need for robust surveillance systems for these healthcare associated infections. Patients undergoing coronary artery bypass grafting (CABG) are at a greater risk for infection due to their relatively older age and the presence of comorbid conditions like diabetes mellitus and obesity.
Objective: To establish the adult cardiothoracic surgical site infections registry to determine adult surgical site infection (SSI) rates and study impact of quality improvement initiatives on SSI rates.
Methods: The Adult Cardiothoracic SSI registry was developed at Armed Forces Institute of Cardiology and National Institute of Heart Disease, Rawalpindi, Pakistan. Monthly SSI rates were monitored for both CABG and valvular heart surgeries inclusive of chest and leg SSIs instituted to control the increased SSI rate in October 2014 after a multidisciplinary approach.
Results: A total number of 1341 cardiac surgeries were carried out and the cumulative SSI rate was 1.7% (n=23) for a period of one year i.e. August 2014 to August 2015, The SSI rate for chest infections was 22% (n=6) and for leg wound (harvest site) infections was 78% (n=17). There was an increase in SSI rate 5% (n= 04) during October 2014. After process improvements the rate declined to 1% in November 2014 and has remained less than or equal to 2% as of August 2015.
Conclusion: A high SSI rate was investigated and multi-modal process improvements and infection control measures were implemented, leading to a decrease in SSI rate from 4% to 1%.
Ahmed Mostafa
Ain Shams University, Egypt
Title: Review of sixty tracheal resections and anastomosis. A seven year experience of a tertiary egyptian referral institute
Time : 12:45-13:15

Biography:
Dr Ahmed MOSTAFA completed his Thoracic Surgery MD in 2009 from Faculty of Medicine- Ain Shams University. He got his pre MD training in France and worked at reputed hospitals such as HEGP-Hôpital Européen Georges-Pompidou, Tenon Hospital. He acquired the MRCS, and he is GMC registered. He has special interest in Airway Surgery. The division of thoracic surgery at Ain Shams University hospitals has quadrupled its annual number of tracheal surgeries since 2009 due to the persistent adoption of the aforementioned management
Abstract:
Introduction: Tracheal stenosis is one of the major complications following prolonged endotracheal intubation. Tracheal resection and anastomosis has proved to be the best solution for this serious problem. This study aims to review the experience of our institute in 7 years with patients presenting with postintubational tracheal stenosis.
Methods: A retrospective study was performed in the period between January 2009 to January 2016. This study involved patients who presented to Ain Shams University Hospitals with postintubational tracheal stenosis, and who underwent tracheal resection and anastomosis as a primary treatment.
Results: We operated upon 60 patients. We excluded glottic stenosis pathology, and patients with major co-morbidities with tracheostomies or stents as definitive treatment . Patients included 42 males (70%), 18 females (30%). Mean age was 28.35 (ranging from 2 to 72 years). At presentation, 45 patients ( 70%) had previous endoscopic dilataions, 38 patients (63.3%) had tracheostomies, 19 patients ( 31.6%) had history of tracheal stenting. Seventeen patients (28.3%) had cricotracheal resections (CTR) for subglottic stenosis. Cervicotomy was sufficient in 41 patients (68.3%), additional manubriotomy was needed in 15 patients (25%), while full sternotomy was done in only 4 patients (6.6%). All patients were given a chance for immediate postoperative extubtion. Anastomotic success rate was (96.6%). In hospital mortality was (1.6%).
Conclusion: Tracheal resection and anastomosis proves to be a safe and satisfactory option for postintubational tracheal stenosis. This intervention must be applied widely in developmental countries where there is frequent rush for tracheostomies, and abuse of tracheal stenting and dilatation. Quality of life improves dramatically following an effective surgery.

Biography:
She has completed her Medical degree (Professional Doctorate) at the age of 26 years from Guilan University of Medical Sciences. She has 5 published and 3 under publish articles. She is the reviewer of the Journal of Biology and Today`s World (An International Biomedical Journal).
Abstract:
Background: Nowadays, percutaneous coronary intervention (PCI) is the most commonly used nonsurgical procedure which restores blood flow to the heart tissue. Such procedures may stimulate myocardial injury and release of myocardial necrosis biomarkers. Although higher levels of cardiac troponins (cTns) are associated with later adverse events, the prognostic importance of the lower levels of cTns, especially highly sensitive assays, is still a matter of controversy.
According to the above points, in the present study, we aimed to assess the prognostic power of mild to moderate elevations in hs-cTnT levels (as an indicator of periprocedural myocardial necrosis) for predicting the one-year outcome of PCI.
Methods and Results: In the present study, all the patients undergoing elective PCI between March 2011 and April 2013 at Tehran Heart Center were followed up. Based on our inclusion and exclusion criteria, finally, 2309 patients were qualified for the study. For measuring hs-cTnT, three blood samples were drawn: the first immediately before the beginning of PCI (baseline), the second 6 h after PCI, and the last 12 h after PCI. The hs-cTnT levels were analyzed using Elecsys 2010 analyzer and major adverse cardiac events (MACE) were assessed one month and one year after the procedure. Based on the pre- and post-procedural hs-cTnT levels, the patients were divided into three groups. But, the differences between the three hs-cTnT groups in terms of frequencies of MACE were not significant.
Conclusions: This prospective study demonstrated no association between mild to moderate elevations in hs-cTnT after PCI and one-year MACE.
Adel Kamel Abdel Malek
Assiut University, Egypt
Title: Implication of protein restriction on the developing heart of albino rat
Biography:
To be updated soon...
Abstract:
Background: Protein malnutrition has become an alarming problem in developing countries and refugee camps.
Aim of the work: The present work aims at studying the effects of maternal protein malnutrition on the structure of the heart of their off-springs.
Material and methods: 20 adult female albino rats were divided into two groups; the first group was fed normal protein diet contained 20% casein and considered as control. The second group were fed low protein diet with 9% casein and considered the experimental group. All breeder rats were habituated to their respective diets for two weeks before mating, during pregnancy and lactation. Hearts of the pups were examined at birth and at the age of one month.
Results: Hearts of pups of undernourished mothers showed cardiac myocytes with fractures of and cytoplasmic vacuulations. There was mitochondrial swellings and dehescience of the intercalated discs.
Conclusion: Changes in the structure of cardiac muscle fibers as a result of protein undernutrition is a potential insult that might lead to irreversible derangement in contractile functions of the heart.
Nattapong Thaiyanurak
Siriraj Hospital, Thailand
Title: Prevalence of anatomical aortic arch variants in Thai patients undergoing thoracic aorta computed tomography angiogram
Time : 14:45-15:15

Biography:
Dr. Nattapong Thaiyanurak graduated his MD from College of Medicine, Rangsit University, Bangkok. He completed his residency in internal medicine and cardiology fellowship training from Siriraj Hospital, Mahidol Universtiy, Bangkok. He is currently the cardiologist at the Lampang Hospital and devotes his time in teaching medical students of Lampang Hospital Medical Education Center, Chiang Mai University.
Abstract:
Yanal F. Al-Naser
Queen Alia Heart Institute, Jordan
Title: 35 years off warfarin-Standing the “Test “or “Challenge†of time?
Time : 15:15-15:45
Biography:
Yanal Al-Naser is a consultant cardiac surgeon from Amman-Jordan. He graduated from University of Jordan in 1999 and was awarded the Jordanian boards in general surgery (2004) and cardiac surgery (2009). He was trained in Manchester –England as an adult cardiac surgeon and finished his training in 2012. He became a consultant adult cardiac surgeon in 2012 at Queen Alia Heart Institute in Jordan. He has a number of publications, and is a member of the Jordanian Cardiac society and the Royal College of Surgeons in the UK.
Abstract:
A 46 year old female patient, with no medical illnesses was referred to my clinic with effort intolerance and palpitations of four years duration. Her history dates back to when she was 11 when she had an Aortic and Mitral valve replacement due to rheumatic causes, she had a size 19mm bileaflet mechanical aortic valve and a size 27mm bileaflet mechanical mitral valve. She was started on warfarin and took it for three months of her life as documented by her family members and follow up notes till she decided to stop it. She stated that she took no medications at all and was completely asymptomatic, she got married and had three children, all a normal vaginal delivery aided by a mid wife at home. Her 2DECHO showed a grade three para-leaking aortic and mitral valves, and was referred to me for a redo AVR and MVR 35 years later, being off warfarin for all that period and was asymptomatic for 30 years and never had a stuck valve. Her coagulation profile was normal, with an INR of 1, I operated on her and found a rim of pannus surrounding the valves, but the leaflets were mobile. I replaced both valves using St Jude size 21 Aortic Valve and size 29 Mitral valves, both mechanical. There are a few cases described in literature about mechanical valves with no warfarin, but I believe this is one of those with the longest –off warfarin- history.
Elisabet Berastegui
Hospital Universitari Germans Trias i Pujol, Spain
Title: Creating a new and simply frailty score for predicting postoperative morbidity in cardiac surgery
Time : 15:45-16:15

Biography:
Elisabet Berastegui completed her studies of Medicine in Barcelona University- Hospital Clinic. She completed her training in Cardiac Surgery in Hospital Vall Hebron where she got her Certificate of research aptitude: Fallot Tetralogy ; Right ventricular remodelling after pulmonary valve replacement in 2010. She works like staff in Hospital Germans Trias I Pujol where is working in areas of frailty and risk, ( Doctoral Programm. Development of Thesis in Autonoma Barcelona University. She is enrolled in differente studys ( PERSIST TRIAL ) and is Coordinator of Spanish PLIAR REGISTER, ( for sutureless prosthesis)
Abstract:
Ageing and elderly people have greater risk. Physical state and frailty status represent an important risk and must be considered before cardiac surgery. More than one third of current surgeries are performed in patients older than 70 years; This is a factor to keep on mind in our routine evaluation. Currently an accepted definition for frailty is not well established. It has been considered as a physiological decline in multiple organ systems, decreasing the patient’s capacity to withstand the stresses of surgery and disease. The aim of our study was to determinate a correlation between preoperative features and the morbidity after cardiac surgery in aortic valve replacement population.
Methods. We selected the 70 years old patients or older who underwent an elective aortic valve replacement. We collected prospectively all preoperative features and frailty traits (Barthel Test; Gait Speed test, Handgrip) also taking into account blood parameters like albumin level and hematocrit previous to the surgery, hospital admissions within 6 months, and we analyze the demographics and medical history of the patients. We compare patients who undergo to stented prosthesis, sutureless or TAVI procedure.
Image
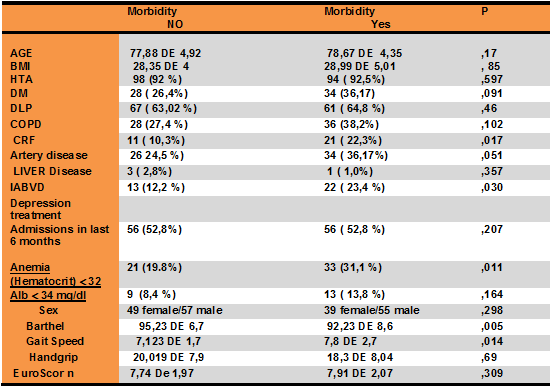
(BMI body mass index, HTA hypertension, DM diabetes mellitus, COPD Pulmonary obstructive disease, IRC chronic renal failure, DLP dyslipidemia, IADL Independence activities daily living)
Results: Two hundred patients were enrolled. The mean age was 78 years all. The predicted mortality with Logistic euroScore I was 12,8% with a real mortality lower than expected (3,5%). Pre-surgery frailty in our population was associated with a Gait Speed higher of 7 seconds, Barthel less of 90%, anemia with Hematocrit <32%, albumin level< 3,4g/dl, chronic renal failure, preoperative re-admission and artery disease. The TAVI group had higher morbidity, no differences statistically significant between Stented and sutureless prosthesis group. Frail individuals had longer hospital stays, readmissions and respiratory/ infectious complications. The mortality at 6 months /one year follow up was 4,1 % /0 % respectively; and morbidity ( pacemaker implant, respiratory events, readmission); at 6 months /one year of follow up was 13,47 % to 3%.
Conclusions: Elderly and frailty population present more complications after a cardiac surgery. A simple frailty score must be considered in cardiac population to avoid increased morbidity.
Poster Presentations 16:30-17:30
Ersöz Gonca
1Bulent Ecevit University, Turkey
Title: A pharmacological study of a new spiro-cyclic benzopyran activator of the cardiac mitoKATP channel on ischemia/reperfusion-induced ventricular arrhythmias

Biography:
Ersöz Gonca has completed his PhD in 2008 from Abant Ä°zzet Baysal University and Post-doctoral studies from Robert Gordon University, the Institute of Health and Welfare Research in 2012. He is studying ischemia/reperfusion-induced ventricular arrhythmias and myocardial injury. He has been conducting his researches in Bülent Ecevit University, Biology Department since 2009.
Abstract:
Background/Introduction: 4’-(N-(4-acetamidobenzyl))-2,2-dimethyl-2,3-dihydro-5’H-spiro [chromene-4,2’-[1,4]oxazinan]-5’-one (compound A) was synthesized as a new spiro-cyclic benzopyran activator of the cardiac mitochondrial ATP-dependent potassium (mitoKATP) channels. A previous study showed the anti-ischemic properties of Compound A.
Purpose: This study was performed to research the effect compound A on ischemia/reperfusion (I/R)-induced ventricular arrhythmias. In our previous study, we suggest that both mitoKATP channel activation and sarcolemmal ATP-dependent potassium (sarcKATP) channel inhibition confer protection against I/R-induced arrhythmias; therefore, we also aimed to test the hypothesis that a combination of mitoKATP channel activation and sarcKATP channel inhibition may be even more effective at decreasing ventricular arrhythmias.
Methods: We performed myocardial I/R by ligating the left main coronary artery for 6 minutes followed by loosening the bond at the coronary artery for 6 minutes in anesthetized rats. The experimental groups were as follows: (1) Vehicle control, (2) Compound A (3 mg/kg) (3) Compound A (10 mg/kg.) (4) Diazoxide (5) HMR 1098 (6) Compound A (10 mg/kg)+HMR 1098 and (7) Diazoxide+HMR 1098 group.
Results: Compoud A at a dose of 10 mg/kg decreased both the arrhythmia score and the total length of arrhythmias (P<0.01). Diazoxide at a dose of 40 mg/kg, a selective mitoKATP channel opener as a reference drug only decreased the total length of arrhythmias (P<0.01). Compound A at a dose of 10 mg/kg was more effective at decreasing the duration of arrhythmias than a dose of 3 mg/kg of compound A and diazoxide. The combination of both diazoxide and compound A with HMR 1098, a selective sarcKATP channel blocker, did not exhibit any additive or synergic effect on the antiarrhythmic effect of each drug alone.
Conclusion(s): These results reveal that compound A may have a dose-dependent antiarrythmic effect, which is more pronounced than the antiarrhythmic effect of diazoxide. Both mitoKATP channel activation and sarcKATP channel inhibition at the same time may not reveal any additive antiarrhythmic effect on I/R-induced arrhythmias.
Anton Cherepov
Federal Research Clinical Center, Russia
Title: Possible mechanisms of peripheral blood pressure adaptation to simulated chronic hypogravity

Biography:
Mr. Anton Cherepov graduated from Medical-Biology Faculty (Biochemistry department) of N.I.Pirogov Moscow Medical Institute in 1989. His first research dealt with the role of lipid peroxidation in Parkinson diseases at the Institute of General Pathology and Pathophysiology, Russian Academy of Medical Sciences. Then he studied immediately-early genes expression in learning and memory on the model of filial imprinting in chicks and other learning models in mice at P.K.Anokhin Institute of Normal Physiology, Russian Academy of Medical Sciences. His current research interest involves methodological approaches for evaluation of specific and non-specific responses of human organism under normal and extreme conditions
Abstract:
Human adaptation to extreme conditions primarily involves the basic vital systems of the body. The aim of our study was to analyze the mechanisms of adaptation of the cardiovascular system to simulated conditions of space flight and stay on the lunar surface.
Hypo- and microgravity was simulated using orthostatic and antiorthostatic hypokinesia, respectively (bedrest at different angles: -6° and +9.6°) and was carried out on volunteers in hospital setting.
Analysis of blood pressure variability (BPV) revealed significant increase in the systolic BPV by 8 day in head-down bedrest group (HDBRG) and return of these parameters to baseline values by day 21. Analysis of the frequency components of systolic BPV spectrum in HDBRG showed that the main contribution to the total spectral power on day 8 was made by the very-low-frequency component. At the same term, we observed a pronounced increase in the very-low-frequency component of heart rate variability (HRV) in HDBRG in comparison with that in head-up bedrest group (HUBRG). Coincidence of these changes may indicate that significant contribution into adaptation is made by central neural mechanisms that are activated during the first week of simulated microgravity. The diastolic BPV was markedly changes by day 21 in both experimental groups in comparison with baseline values, primarily at the expense of very-low-frequency component of BPV. In HRV, no similar changes were observed by day 21 of the experiment. These findings probably attest to predominance of local mechanisms of vascular tone regulation not directly related with the autonomic control.
Riccardo Turri
Mirano General Hospital, Italy
Title: Multi-district atherosclerotic disease: mid-term outcome of hybrid or totally endovascular coronary and carotid revascularization

Biography:
Riccardo Turri graduated with the best ratings at Padua University in Italy; he was always engaged in studying and applying into invasive cardiology and acute cardiologic care. His competences include coronary angioplasty, bifurcation lesions, coronary imaging and functional assessment, limb and BTK angioplasty. In the last 3 years he worked as an interventional cardiologist at Mirano General Hospital, near Venice, in Italy.
Abstract:
Background: The socio-economic impact of multi-district atherosclerotic disease is elevated for frequent hospitalizations and morbidity/mortality.
Aim: Assess clinical characteristics, angiographic findings, therapeutic strategy and outcome of patients hospitalized with a concomitant diagnosis of coronary artery and carotid obstructive diseases.
Methods: We evaluate all patients hospitalized from 2006 to 2012. Revascularization strategies were hybrid (carotid stenting CAS and cardiac surgery CABG) or totally endovascular (coronary angioplasty PCI and CAS).
Results: 107 patients enrolled, 42.1% hospitalized for carotid obstructive disease (groupA), 57.9% for coronary artery disease (groupB). Patients were treated with PCI and staged CAS in 28% of cases (15.6% in groupA, 37.1% in groupB), with CAS and staged PCI in 21.5% of cases (46.7% in groupA, 3.2% in groupB), with CAS and simultaneous CABG in 39.3% of cases (24.4% in groupA, 50% in groupB) and with PCI and simultaneous CAS in 11.2% of cases (13.3% in groupA, 9.7% in groupB). 30-days results: mortality 0%, major/minor stroke 3.7% (2.2% in groupA, 4.8% in groupB), myocardial infarction 2.8% (0% in groupA, 4.8% in groupB), major bleeding 5.6% (2.2% in groupA, 8.1% in groupB). Major bleeding affected only patients with acute symptoms and 11.9% of patients following CABG. Follow-up results: cardiovascular mortality 4.7% (2.2% in groupA, 6.5% in groupB), all-cause mortality 2.8% (4.4% in groupA, 1.6% in groupB), stroke 0.9% (2.2% in groupA, 0% in groupB), myocardial infarction 2.8% (4.4% in groupA, 1.6% in groupB). The only predictor of mortality at follow-up was the inhospital stroke (HR 7.6 for all-cause mortality, 16.5 for cardiovascular mortality).
Conclusions: Patients with concomitant coronary artery disease and carotid obstructive disease were treated with a high procedural success, following a hybrid or totally endovascular revascularization. Patients hospitalized in an acute setting have more strokes and bleedings at 30 days; these patients need therefore most careful assessment and treatment.
Rawa Delshad
Hawler Medical University, Iraq
Title: Utility of cardiac biomarkers in combination with exercise stress testing in patients with suspected ischemic heart disease
Biography:
To be updated soon...
Abstract:
Eighty patients with suspected ischemic heart disease were enrolled in the present study. They were classified into two groups: patients with positive exercise stress test results (n=40) and control group with negative exercise stress test results (n=40). Serum concentration of troponin I, Heart-type Fatty Acid Binding Protein (H-FABP) and Ischemia Modified Albumin (IMA) were measured one hour after performing stress test. Enzyme Linked Immuno-sorbent Assay was used to measure both troponin I, H-FABP levels, while IMA levels were measured by albumin cobalt binding test. There was no statistically significant difference in the mean concentration of troponin I between two groups (0.75±0.55ng/ml) for patients with positive test result vs. (0.71±0.55ng/ml) for negative test result group with P>0.05. Contrary to our expectation, mean IMA level was slightly higher among control group (70.88±39.76U/ml) compared to (62.7±51.9U/ml) in positive test result group, but still with no statistically significant difference (P>0.05). Median H-FABP level was also higher among negative exercise stress testing group compared the positive one (2ng/ml vs. 1.9ng/ml respectively), but failed to reach statistically significant difference (P>0.05). When quartiles model used to explores the possible association between each study biomarkers with the others; serum H-FABP level was lowest (1.7ng/ml) in highest quartile of IMA and lowest H-FABP (1.8ng/ml) in highest quartile of troponin I but with no statistically significant association (P>0.05). Myocardial ischemia, more likely occurred after exercise stress test, is not capable of causing troponin I release. Furthermore, an increase in H-FABP and IMA levels after stress test are not reflecting myocardial ischemia. Moreover, the combination of troponin I, H-FABP and IMA after measuring their post exercise levels does not improve the diagnostic utility of exercise stress test enormously.
Khizar Khan-Mahmood
Colchester General Hospital, Colchester, Essex, UK
Title: The root of all evil: A case reeport documenting the presentation of an aortic root abscess in a 26 year old gentelman

Biography:
Dr Khan-Mahmood completed his MBBS age 24 from Barts and the London School of Medicine and Dentistry, Queen Mary University of London. During this time, he intercalated in Oral Biology, and gained a BSc (first class honours). He graduated with a MBBS and BSc (hons). Dr Khan-Mahmood went on to complete foundation training at Addenbrookes Hospital, Cambridge University Trust. He took a year out of training, to set up various business ventures and to travel, volunteering in health services around the world. Currently a Core Medical Trainee at Colchester General Hospital, Essex, with a keen specialist interest in Cardiology.
Abstract:
Background: Aortic root abscesses are a complication of infective endocarditis. A devastating disease with high morbidity and mortality leading to complications such as atrioventricular septal destruction, even death.
Objectives
Demonstrate importance of coordination between health professionals.
Highlight importance of examination, investigation and senior support.
Demonstrate how young patients maintain good physiological reserve masking severe infection.
Materials and Methods:Literature search. Patient consented.
Results: TTE demonstrated normal left ventricular function, EF 50-55%, and an unusual aortic valve anatomy with significant aortic regurgitation.
Blood cultures were negative; IV amoxicillin and IV gentamycin were commenced.
TOE revealed thickened aortic leaflets and moderate aortic regurgitation, suggesting infective endocarditis. Aortic root was suspicious of an aortic root abscess.
Patient continued to spike temperatures. Antibiotics changed to gentamycin, vancomycin and rifampicin. Case discussed at cardiothoracic centre. Patient was diagnosed with aortic root abscess, transferred and underwent an aortic root and mechanical valve replacement.
Specimen was culture negative, PCR positive for Staphylococcus lugdunensis. Post-operatively commenced on warfarin and a four month course of rifampicin and daptomycin.
Conclusions: Young patients mask a multitude of sins and present with subtle symptoms given good physiological reserve. The root of all evil was the aortic root.
Clear, precise, detailed history and review of results highlights serious cases early, benefitting from prompt review.
Aortic root abscess is a serious complication of infective endocarditis and should always be considered if symptoms do not respond to treatment after 72hrs.
Specialist input is useful and important. Advances in cardiac imaging allows useful investigative correlation, with the ultimate treatment option being cardiothoracic surgery.
Ygal Plakht
Ben-Gurion University of the Negev, Israel
Title: Acute myocardial infarction: The association of changes in K+ levels and in-hospital mortality of patients with acute myocardial infarction
Biography:
To be updated soon...
Abstract:
Background: serum potassium levels (K, mEq/L) of patients with acute myocardial infarction (AMI) were found to be associated with short- and long-term outcomes. Nevertheless, significant fluctuations in K have been reported during the acute phase of an AMI.
Aims: to evaluate the association between K changes during the hospitalization and in-hospital mortality of patients admitted with AMI.
Methods: AMI patients hospitalized in a tertiary medical center, between 2002-2012, for 3 days or longer, were studied. Based on K levels during the hospitalization, the following parameters were calculated: minimal, maximal, range (maximal-minimal) and fluctuation (the gap between two consecutive K levels). The latter parameters were calculated for every K throughout the hospitalization. The associations between the parameters and outcome were assessed using generalized estimating equations model, adjusted to baseline patients’ characteristics and results of other routine laboratory tests (i.e. Sodium, Creatinine and Glucose).
Results: overall 16,596 admissions of 12,176 patients were included (age 67.8±13.9 years, 66.6% males), and 111,457 K results registered. Overall, patients discharged alive from 15,564 admissions, with an in-hospital mortality rate of 6.2%. Compared with survivors, in-hospital mortalities had higher mean K (4.4±0.8 vs. 4.3±0.6), higher rate of fluctuation or range ≥0.4 (p<0.001 for each). Minimal K throughout the first 48 hours was significantly more prevalent among survivors compared to deceased (41% vs 25% p<0.001). In a multivariate analysis the following parameters were found to be independent prognostic marker for mortality: K<3.9 (adjOR=1.22) or K>4.8 (adjOR=1.17), range ≥0.8 (adjOR=1.53) and minimal K during the first 2 days of admission (adjOR=1.49). Furthermore K fluctuation ≥0.4 was associated with increased mortality within the following 72 hours (adjOR=1.37), (p<0.001 for each).
Conclusions: changes in K, in addition to extreme values throughout an admission of AMI patients are strong prognostic markers of in-hospital mortality. Close monitoring of K in addition to further evaluation of mechanisms and interventions in K are in order.
Abdullah Nabi Aslan
Ankara Ataturk Education and Research Hospital, Turkey
Title: Coexistence of gitelman syndrome and hypertrophic obstructive cardiomyopathy in a pregnant woman

Biography:
Abdullah Nabi ASLAN has completed his PhD at the age of 25 years from Marmara University and postdoctoral studies from Ankara Ataturk Education and Research Hospital,Department of Cardiology. He is a specialist of cardiology. He has published more than 30 papers in reputed journals and has been serving as an editorial board member of Clinical Cardiology Updates journal. I also take a role of reviewer in some reputed journals and like my job too much.
Abstract:
A 34-year-old woman with GS presented at 20 weeks gestation with the complaints of palpitation, fatigue and presyncope. This was her first pregnancy. Her initial diagnosis of GS had been confirmed 4 years ago based on clinical presentation and laboratory data. She was maintained on oral electrolyte replacement with oral potassium chloride and magnesium citrate were prescribed and the course of the pregnancy. At physical examination there was a grade 3/6 systolic ejection murmur maximally heard at apical focus of the heart. Blood pressure was 80/50 mmHg and laboratory test showed a serum potassium value of 2.5 mmol/L (normal 3.5-5.1), a serum calcium value of 10.2 mg/dL (normal 8.6-10.0) and a serum magnesium level of 1.4 mg/dL (1.6-2.6) were noted. Blood gas analysis showed metabolic alcalosis with a pH of 7.495 (normal 7.380-7.460), pCO2 of 35.6 (normal 32-46) and HCO3 of 34.1 mmol/L (normal 22-26). Serum creatinine, urea and remainder ionograms were normal. Electrocardiogram (ECG) showed normal sinus rhythm with a rate of 67 beats per minutes and remarkable ST-T changes at inferior and precordial derivations. There was also a prolonged QT interval (490 ms) (Fig 1). Echocardiography determined a hypertrophic obstructive cardiomyopathy (HOCM) with a septal thickness of 2.1 cm and posterior wall thickness of 1.1 cm (Fig.2a) and a resting gradient of 30 mmHg (Fig. 2b). There was also systolic anterior motion in mitral valve creating a mild degree of mitral regurgitation (video). Risk of SCD at 5 years was calculated as 2.93%. Because the patient was pregnant, the cardiology, gynecology and pediatric departments organised a council whether the patient will maintain the pregnancy or not. The common consensus was close follow-up and if needed termination. At follow-ups, the pregnancy was continued without any complication with a born healhy daughter.
Muhammad Asad Sheikh
Peterborough City Hospital, UK
Title: Cortical blindness post coronary angiogram, a rare but frightening complication

Biography:
Dr. Muhammad Asad Sheikh has completed MBBS degree form Allama Iqbal Medical College, Pakistan and has been in training in UK for last 5 years. He has speacial interest in Cardiology and has done many presentations and teachings on various topics in cardiology.
Abstract:
Cortical blindness is a rare but frightening complication following coronary angiogram probably due to contrast penetration in occipital lobes in susceptible individuals.
A case report of 82 years old man was admitted with collapse. Investigations showed NSTEMI with T wave inversion in lateral leads and Troponin rise. Severe LCX disease was found on coronary angiogram, which was stented with DES with good angiographic results. Patient became blind 30 minutes after the procedure.
Clinical examination showed diminished visual acuity to light perception bilaterally. Light reflex and fundoscopy was unremarkable. Motor, sensory & cerebellar systems were normal. No other abnormality was detected.
CT head scan showed bilateral contrast enhancement in the occipital lobes. Patient was not considered for thrombolysis due to symmetrical bilateral focal neurological presentation, which is uncommon in cerebrovascular accidents. Patient had a partial recovery of vision while in observation ward and had complete recovery within 24 hours. Patient remained asymptomatic at 2 months follow-up post discharge.
A clinical diagnosis of “cortical blindness” was made, however it was thought to be unlikely due to thrombo-embolism secondary to cardiac catheterization so thrombolysis was withheld (symmetrical bilateral focal neurological lesions are very uncommon in cerebrovascular accidents).
A quick literature search showed case reports of cortical blindness linked with coronary angiography and such blindness almost always spontaneously recovers in hours to days time.
Although the exact cause is unknown it is postulated that there is a direct neurotoxic effect of contrast in occipital cortex potentiated by prolonged lying position during coronary angiogram.
Other possible mechanisms includes spasm of the posterior cerebral arteries, dissection of the aortic arch, and contrast-induced hypotension.
Abdullah Nabi Aslan
Ankara Ataturk Education and Research Hospital, Turkey
Title: Impact of coronary artery dominance on P wave dispersion

Biography:
Abdullah Nabi ASLAN has completed his PhD at the age of 25 years from Marmara University and postdoctoral studies from Ankara Ataturk Education and Research Hospital,Department of Cardiology. He is a specialist of cardiology. He has published more than 30 papers in reputed journals and has been serving as an editorial board member of Clinical Cardiology Updates journal. I also take a role of reviewer in some reputed journals and like my job too much.
Abstract:
Background: P-wave duration and dispersion has been proposed as being useful for the prediction of paroxysmal atrial fibrillation (AF). The aim of this study was to investigate the effect of coronary artery dominance on P wave duration and dispersion.
Design and Methods: The study population included 194 patients with left dominant (LD) circulation and 200 age and gender-matched controls with right dominant (RD) circulation and without coronary artery dissease based on invasive coronary angiography findings. The electrocardiogram of each patients was obtained upon admission to hospital and evaluated by two cardiologists blinded to the angiographic results of the patient. P-wave dispersion (PWD) was defined as the difference between the maximum and minimum P-wave duration. Statsitical analyses were performed using SPSS v17.0 statistical software package.
Results: PWD was shown to be significantly prolonged in patients with LD circulation compared to controls with RD circulation (48 ± 14 ms vs 33 ± 15 ms, p = 0.001). P wave duration was similar between the groups (p = 0.124). Moreover, there was positive correlation between PWD and age (r: 0.502, p= 0.009), left ventricular (LV) mass (r: 0.614, p= 0.001), LV mass index (r: 0.727, p< 0.001) and left atrium (LA) diameter (r: 0.558, p= 0.003) in LD circulation patients. Multivariate logistic regression analysis determined age, LV mass index, LA diameter and LD circulation as independent predictors of prolonged PWD.
Conclusions: LD circulation could lead to an increased risk of AF through prolonged PWD. We recommend follow-up of these patients to assess the development of AF in the future.
Nadeeja Himanthi Gamalath Seneviratne
The National Hospital of Sri Lanka, Sri Lanka
Title: Factors associated with survival of post Coronary Artery Bypass Graft (CABG) patients registered in cardiology Unit, National Hospital Sri Lanka (NHSL)

Biography:
Dr. (Mrs) NHG Seneviratne, MBBS (Sri Lanka), MD Medicine (Colombo). – She obtained MD Medicine from Post Graduate Institute of Medicine, University of Colombo in 2013. Currently she is undergoing post doctoral training in Cardiology at Institute of Cardiology NHSL. She has published four papers in local forums and one poster presentation which won the gold medal for best poster in 2010. She has done oral and poster case presentations at Asian Interventional Cardiovascular Therapeutices Congress 2015, Dhaka, Bangladesh. She works as a sub inspector in ODYSSEY and TRIUMPH multi centre clinical trails and a resource person in frailty study.
Abstract:
CABG is one of the treatment options for the patients with coronary artery disease (CAD). This study was aimed to describe survival up to occurrence of cardiac events and factors associated with them among CABG patients at NHSL.
Retrospective analytical study was carried out among the patients who had undergone CABG at least one year before the date of data collection. Cardiac event was defined as new occurrence of any condition namely; unstable angina (UA), ST elevated myocardial infarction (STEMI), non ST elevated myocardial infarction (NSTEMI) and heart failure (HF). Survival was assessed up to the defined cardiac events.
The sample (n=421) consists 74.6% males and mean age was 63.16years (SD = 7.86). Event rates were UA (13.3%), STEMI (0.5%), NSTEMI (3.1%) and heart failure (8.6%). Kaplan-Mayer survival analysis revealed the probability of survival at 5 years was 79.6% (CI 0.781-0.871) and 10 year was 58.1% (CI 0.516- 0.688). Cox regression revealed significant associations with age (HR- 0.973, p=0.023), family history (FH) of hypertension (HR-2.2, p=0.044) compared to negative family history and activities of daily living (ADL) independency (HR=0.16, p= 0.011) compared to the ADL dependency.
CABG surgery reserves its own place in management of CAD. Sri Lankan survival data of CABG patients seems to be similar to other countries of the world. Age, status of ADL prior to CABG and family history of hypertension were significantly associated with survival.
Withma Muthukumara
Lancaster Medical School, UK
Title: Case-based evaluation of the effectiveness of PCI and CABG in the management of multi-vessel Coronary Artery Disease
Biography:
To be updated soon...
Abstract:
Introduction: Multi-vessel coronary artery disease (CAD) can give rise to numerous disabling symptoms such as angina, shortness of breath (SOB) and fatigue, considerably impairing quality of life (QoL). Percutaneous coronary intervention (PCI) and coronary artery bypass surgery (CABG) have been developed to overcome these and increase life expectancy. The controversy over treatment preference has been a historical battle which CABG has dominated. However, the development of drug eluting stents (DES) is reducing the margin of difference in symptom improvement between the two interventions, making decisions difficult. Large randomized control trials (RCTs) such as SYNTAX, ARTSI/II and FREEDOM have set out to investigate the outcomes for each treatment and provide recommendations.
Aims: To measure QoL in terms of the symptom experience between 4 patients who had PCI/CABG and recognise the intervention providing the largest relief of symptoms. Additionally, explore the evidence behind PCI and CABG for multi-vessel CAD from RCTs and compare their outcomes with Case findings.
Method: 4 clinical cases, 2 undergoing PCI and 2 undergoing CABG, with multi-vessel CAD were selected. QoL was assessed using the Cardiovascular Limitations And Symptoms Profile (CLASP) questionnaire to explore the severity of symptoms before and after the intervention.
Results: Patients in the PCI group had an overall symptom reduction of 57.9% compared to only 38.9% in the CABG group. The greatest effect was seen in the angina category for PCI and SOB category for CABG, which resulted in a 100% relief of symptoms.
Conclusion: All patients had an improvement in symptoms to some degree, regardless of the type of intervention, but PCI patients had better outcomes across 4 more categories than CABG patients. RCTs report greater relief of symptoms following CABG, which was inconsistent with Case findings. CABG has demonstrated an increase in life expectancy and QoL in patients with SYNTAX scores ≥23 and more severe multi-vessel CAD, especially in diabetic patients, making it the treatment of choice.
