Riccardo Turri
Mirano General Hospital, Italy
Title: Multi-district atherosclerotic disease: Mid-term outcome of hybrid or totally endovascular coronary and carotid revascularization
Biography
Biography: Riccardo Turri
Abstract
Background: The socio-economic impact of multi-district atherosclerotic disease is elevated for frequent hospitalizations and morbidity/mortality.
Aim: Assess clinical characteristics, angiographic findings, therapeutic strategy and outcome of patients hospitalized with a concomitant diagnosis of coronary artery and carotid obstructive diseases.
Methods: We evaluated all patients hospitalized from 2006 to 2012. Revascularization strategies were hybrid (carotid stenting CAS and cardiac surgery CABG) or totally endovascular (coronary angioplasty PCI and CAS).
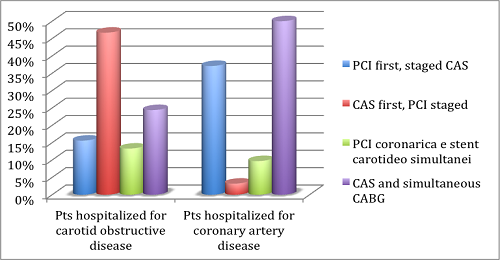
Results: 107 patients were enrolled, 42.1% were hospitalized for carotid obstructive disease (groupA), and 57.9% for coronary artery disease (groupB). Patients were treated with PCI and staged CAS in 28% of cases (15.6% in groupA, 37.1% in groupB), with CAS and staged PCI in 21.5% of cases (46.7% in groupA, 3.2% in groupB), with CAS and simultaneous CABG in 39.3% of cases (24.4% in groupA, 50% in groupB) and with PCI and simultaneous CAS in 11.2% of cases (13.3% in groupA, 9.7% in groupB). 30-days results: Mortality 0%, major/minor stroke 3.7% (2.2% in groupA, 4.8% in groupB), myocardial infarction 2.8% (0% in groupA, 4.8% in groupB), major bleeding 5.6% (2.2% in groupA, 8.1% in groupB). Major bleeding affected only patients with acute symptoms and 11.9% of patients following CABG. Follow-up results: Cardiovascular mortality 4.7% (2.2% in groupA, 6.5% in groupB), all-cause mortality 2.8% (4.4% in groupA, 1.6% in groupB), stroke 0.9% (2.2% in groupA, 0% in groupB), myocardial infarction 2.8% (4.4% in groupA, 1.6% in groupB). The only predictor of mortality at follow-up was the in-hospital stroke (HR 7.6 for all-cause mortality, 16.5 for cardiovascular mortality).
Conclusions: Patients with concomitant coronary artery disease and carotid obstructive disease were treated with a high procedural success, following a hybrid or totally endovascular revascularization. Patients hospitalized in an acute setting have more strokes and bleedings at 30 days; these patients need therefore most careful assessment and treatment.
Image